By Lisa Belanger and Carolyn Ridge

Carolyn and Lisa
One of the most challenging aspects of having cancer is finding someone you can relate to. And who better to understand you than another cancer survivor? This is our story of cancer and friendship.
Lisa’s Story: I was diagnosed with ovarian cancer at the ripe age of 29 on Sept. 12, 2011, upon waking up from surgery to remove what was thought to be a benign ovarian cyst. I was in my final semester of graduate school and nearly a year into the most serious long-term relationship of my life. I had plans to advance my career, settle down with the man I loved, and eventually start a family. Suddenly, those dreams were flipped upside down with three little words: “you have cancer.”
Within a matter of weeks, I started chemotherapy and managed to finish my last semester of my MBA at Boston University, but as my fellow graduates were moving on to bigger and better things with their careers, I was at home, throwing up while my mom made me toast. My boyfriend stuck by my side, but our dream of having a family someday has been challenged as I underwent a full hysterectomy in May 2012. I chose not to harvest my eggs as my doctors advised it would be too risky to delay treatment given the size of my tumor – as large as a grapefruit.
Carolyn’s Story: I was diagnosed with ovarian cancer on June 1, 2012, at the age of 30. While spending the summer in Massachusetts on break from nursing school in Nashville, I began experiencing symptoms of a urinary tract infection. One doctor’s visit, a CT scan, and four days in the hospital turned my world upside-down. Those three little words, “you have cancer,” reversed my role from caregiver to patient as I took a medical leave from nursing school to focus on my treatment. I immediately had surgery before undergoing six months of intense chemotherapy, and was given the “all clear” on Dec. 6, 2012.
Our Story: We met in the spring of 2013 at the young adult cancer support group hosted by Dana-Farber’s Young Adult Program. It was there our friendship blossomed.
We both started attending the support group regularly and quickly learned it was our age, rather than our diagnosis, which helped us connect with other patients. We found in the support group a handful of people to talk to (and cry with – oh boy, did we cry!) about the issues consuming us as 30-somethings trying to find our way in life. We understood each other in ways non-cancer friends couldn’t and would never be able to.
In each other we found someone who had her young life paused, too, along with the same rare, pre-menopausal ovarian cancer diagnosis. We shared not only the same fears and uncertainties about cancer, but also the physical symptoms and side effects. Our friendship began by comparing notes on our treatment plans, what hormone therapy we were taking, our surgery scars, hair loss, and the loss of our fertility (pregnancy was something we had both yearned for as young women). But soon our conversations leaned more towards what other 30-somethings talk about: relationships, dating, jobs, school, family, clothes, cooking. We stopped being cancer friends and started being friends. We grabbed dinner and drinks, sent each other birthday and Christmas cards, even planned a weekend away in Las Vegas together. Sure, cancer is still a topic of conversation, but it’s not the only topic, and it certainly isn’t the most important. And if there is a silver lining to the cloud that is this journey to Hell and back, it is our friendship, and for that we are forever grateful.


 For many patients treated with
For many patients treated with 


 4. Take some “me” time. Many patients and survivors are used to taking care of families, spouses, or tasks at work. However, it’s important to set aside some time that is just for you. Ask yourself when the last time was that you truly had “me” time. You could try leaving for an appointment an hour early to give yourself time to make a stop at a favorite coffee shop, store, or park.
4. Take some “me” time. Many patients and survivors are used to taking care of families, spouses, or tasks at work. However, it’s important to set aside some time that is just for you. Ask yourself when the last time was that you truly had “me” time. You could try leaving for an appointment an hour early to give yourself time to make a stop at a favorite coffee shop, store, or park.







 Karen Fasciano, PsyD
Karen Fasciano, PsyD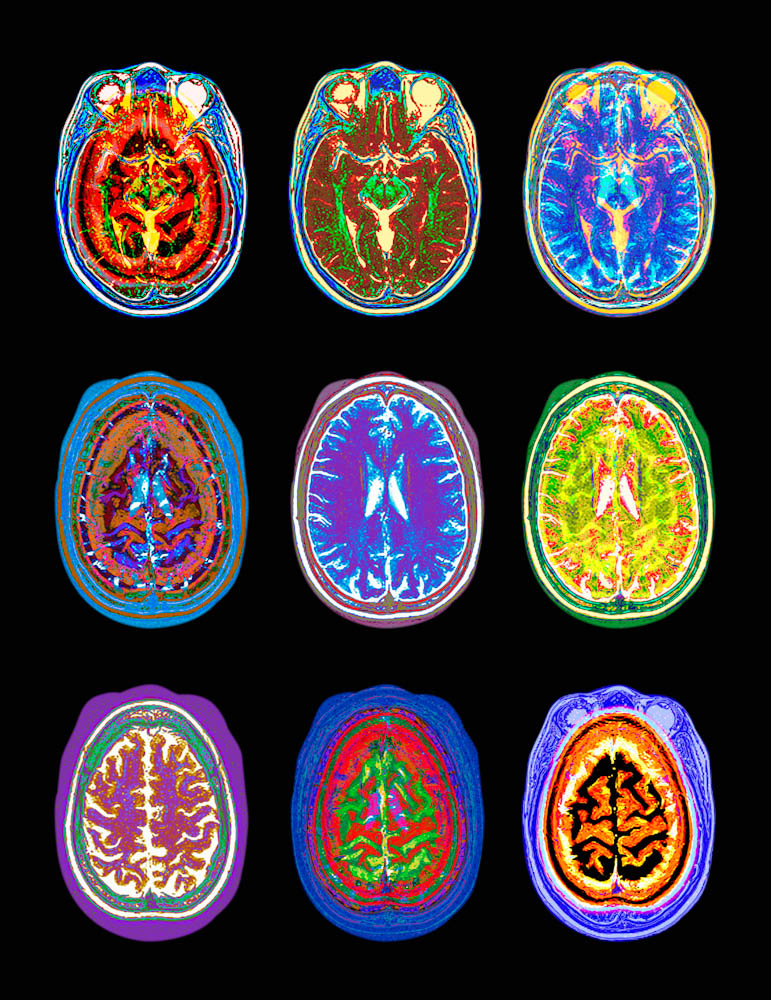 1. What is a glioblastoma?
1. What is a glioblastoma? “It’s common for cancer patients, even if they don’t have full-blown PTSD, to have some of the symptoms of it,” says
“It’s common for cancer patients, even if they don’t have full-blown PTSD, to have some of the symptoms of it,” says 
 Melanin strongly absorbs sunlight and helps to protect the skin from ultraviolet light that damages DNA, which can contribute to the development of cancer. Because people with dark skin have more protective melanin, they are at lower risk of developing melanoma than those with light skin. However, it should be kept in mind that individuals with any skin type can develop melanoma.
Melanin strongly absorbs sunlight and helps to protect the skin from ultraviolet light that damages DNA, which can contribute to the development of cancer. Because people with dark skin have more protective melanin, they are at lower risk of developing melanoma than those with light skin. However, it should be kept in mind that individuals with any skin type can develop melanoma.




 “Other than biology class, I haven’t had the opportunity to do science,” Kate says. “This is the real thing.”
“Other than biology class, I haven’t had the opportunity to do science,” Kate says. “This is the real thing.” “We’re trying to cultivate the next generation of scientists,” Walensky says. “Having the interns in the lab creates a wonderful dynamic. They remind the older students of those early feelings of ‘wow’ about the wonders of science that inspired them to pursue research careers.”
“We’re trying to cultivate the next generation of scientists,” Walensky says. “Having the interns in the lab creates a wonderful dynamic. They remind the older students of those early feelings of ‘wow’ about the wonders of science that inspired them to pursue research careers.” Researchers in the
Researchers in the 


![Behaylu Barry 009[1]-2](http://blog.dana-farber.org/insight/wp-content/uploads/2014/08/Behaylu-Barry-0091-2.jpg)