![Share]()
Close to 100,000 women are diagnosed with a gynecologic cancer in the United States each year. In recognition of Gynecologic Cancer Awareness Month, we’re taking a look at the main types of gynecologic cancers and their symptoms.
Cervical cancer
In cervical cancer, cancer cells form in the tissues of the cervix, the lower, narrow end of the uterus. More than 12,000 new cases are diagnosed in the U.S. each year. Unlike other gynecologic cancers, cervical cancer has a standard screening test, the Pap smear, during which a doctor takes a sample of cells from the cervix. Doctors may also test DNA for the human papillomavirus (HPV), which contributes directly to cervical cancer.
Symptoms of cervical cancer, including vaginal bleeding or unusual discharge, pelvic or back pain, or bleeding after sexual intercourse, may not appear until the disease is advanced. Women who have HPV, many sexual partners, or a weakened immune system, or who smoke cigarettes or had sexual intercourse at a young age, are at a higher risk of developing this disease.
![The Gynecologic Oncology team from the Susan F. Smith Center for Women's Cancers meets regularly to coordinate patient treatment plans.]()
The Gynecologic Oncology team from the Susan F. Smith Center for Women’s Cancers meets regularly to coordinate patient treatment plans.
Endometrial (uterine) cancer
The endometrium is the lining of the uterus, part of which is shed during a woman’s menstrual cycle. About 52,630 women are diagnosed in the U.S. each year, 75 percent who are over the age of 55. Symptoms of endometrial cancer include abnormal bleeding or discharge, difficult or painful urination, pelvic pain, or pain during sexual intercourse. Women who take estrogen without progesterone, are overweight, have diabetes mellitus, or a family history of Lynch syndrome, or who take tamoxifen for breast cancer, are at a higher risk of developing endometrial cancer.
Ovarian cancer
Ovarian cancer can form in the tissue of the ovaries, which produce eggs and female hormones, or in the fallopian tubes, and it accounts for more deaths than any other gynecologic cancer. If women develop symptoms of ovarian cancer, which include abdominal pain, feeling full after eating, and abdominal swelling, they should see their gynecologist or primary care doctor. While there is no single effective screening test for ovarian cancer, pelvic exams, during which a doctor physically examines a woman’s reproductive organs, combined with an ultrasound, blood tests, biopsy, or a CT scan, can help diagnose the disease. The most common risk factors for ovarian cancer include a family history of ovarian and/or breast cancer, as well as other cancers, such as melanoma and pancreatic cancer, the use hormone replacement therapy or fertility drugs, having never had children or infertility, and late onset of menopause.
Gestational trophoblastic tumor
A rare cancer accounting for less than one percent of gynecologic cancers in the U.S., gestational trophoblastic tumor is a disease where cancer cells form in the tissues created in the uterus following conception. These tumors can be difficult to find because they often look like a normal pregnancy; however, if a woman is experiencing abnormal vaginal bleeding or if she is pregnant, but the baby has not moved at the expected time, it may be a sign of trophoblastic disease. Doctors may test for gestational trophoblastic tumors with a pelvic exam, ultrasound, or blood test for the beta-HCG hormone, which is a sign of pregnancy. If a woman has symptoms of a tumor, but no HCG in her blood, it may be an indication of trophoblastic disease.
Vaginal cancer
There are two main types of vaginal cancer. Squamous cell carcinoma is the most common and spreads slowly near the vagina, but may continue to the lungs, liver, or bones. The other main type is adenocarcinoma, which forms in the glandular cells lining the vagina and is more likely to spread to the lungs and lymph nodes. Risk factors for this rare cancer (just 3,170 new cases per year in the U.S.) include being exposed to the drug DES (diethylstilbestrol) before birth, HPV, having a hysterectomy, or being over the age of 60. Women experiencing abnormal bleeding or discharge, pain in the pelvic area, constipation, a lump in the vagina, or pain while urinating or during sexual intercourse should talk to their doctor, who can perform a pelvic exam, Pap smear, biopsy, and other tests to determine the presence of cancer.
Vulvar cancer
Vulvar cancer, which accounts for four percent of gynecologic cancers, forms in a woman’s external genitalia, most often in the outer vaginal lips. One of the main risk factors for vulvar cancer is vulvar intraepithelial neoplasia (VIN), in which abnormal cells grow slowly on the vulvar skin over time. Other risk factors include having HPV or a history of genital warts. Women with vulvar cancer may experience abnormal bleeding or itching, tenderness, lumps or growths, or color changes or growths on the vulvar skin.
Successful treatment of gynecologic cancers depends on recognizing symptoms early and being evaluated by oncologists who specialize in gynecologic cancers. Survival rates for many of these cancers have increased through the years, and researchers from the Gynecologic Oncology Program at the Susan F. Smith Center for Women’s Cancers at Dana-Farber are continuously working on new treatment options, many of which have resulted in innovative clinical trials for these diseases. Learn more about gynecologic cancers, their symptoms, and treatment by visiting the Susan F. Smith Center for Women’s Cancers.





 This year, Sirvis will have a special name to add to her shirt. In July, her 90-year-old mother was diagnosed with
This year, Sirvis will have a special name to add to her shirt. In July, her 90-year-old mother was diagnosed with 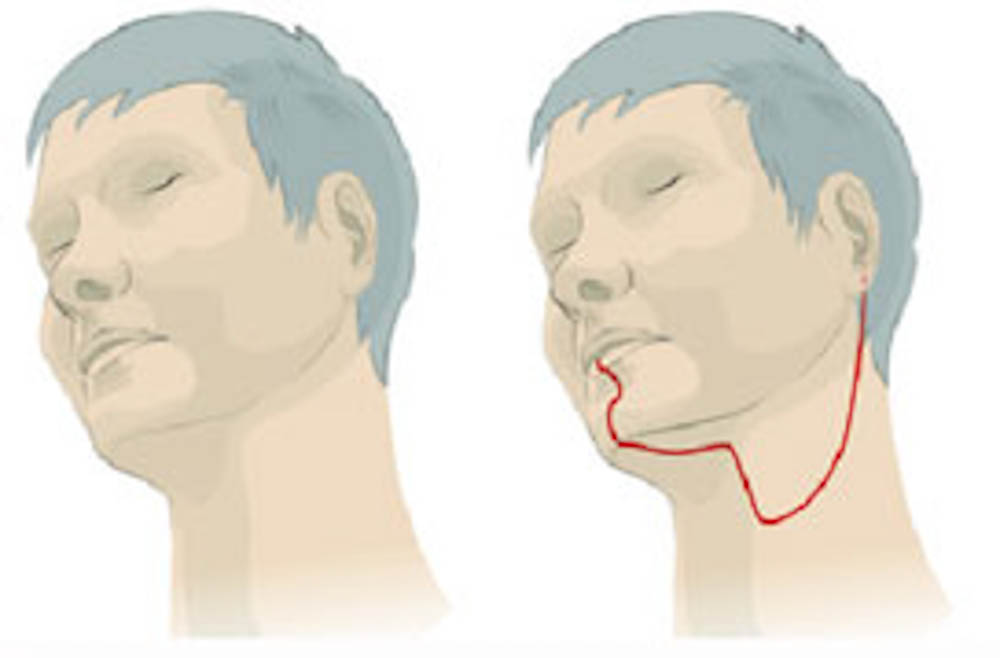


 Both of my parents battled cancer during the same three-year span. The first diagnosis came when I was 13 and the second when I was 14. This disease, as random as it is, chose to favor one of my parents over the other; this past March, my father lost his battle. Between 2011 and 2014, I saw my superhero parents take on a lot of new roles. They shared the role of
Both of my parents battled cancer during the same three-year span. The first diagnosis came when I was 13 and the second when I was 14. This disease, as random as it is, chose to favor one of my parents over the other; this past March, my father lost his battle. Between 2011 and 2014, I saw my superhero parents take on a lot of new roles. They shared the role of 


 What are the risk factors for GTD?
What are the risk factors for GTD?


 Since younger women are generally less aware of their risk and are less likely to be screened,
Since younger women are generally less aware of their risk and are less likely to be screened, 

 I sometimes struggle with my balance. My information processing speed is a little slower than normal. And my overall neurological function can be labored. However, I also participate in horse shows, and made the Dean’s List both semesters I’ve been at Wheaton. I have to give myself more time to do my assignments, and I am frequently working with the dean of disabilities, but my professors and counselors pay close attention and help me keep track of my work.
I sometimes struggle with my balance. My information processing speed is a little slower than normal. And my overall neurological function can be labored. However, I also participate in horse shows, and made the Dean’s List both semesters I’ve been at Wheaton. I have to give myself more time to do my assignments, and I am frequently working with the dean of disabilities, but my professors and counselors pay close attention and help me keep track of my work. More recently, a team at Fox Chase Cancer Center in Philadelphia presented new research showing that low-dose aspirin helps suppress inflammatory pathways that feed prostate cancer cell formation. And another study in 2014 reported that daily aspirin could reduce the risk of ovarian cancer by 20 to 34 percent.
More recently, a team at Fox Chase Cancer Center in Philadelphia presented new research showing that low-dose aspirin helps suppress inflammatory pathways that feed prostate cancer cell formation. And another study in 2014 reported that daily aspirin could reduce the risk of ovarian cancer by 20 to 34 percent.


 Hysterectomy, the surgical removal of the uterus, may be used to treat a variety of
Hysterectomy, the surgical removal of the uterus, may be used to treat a variety of  Typically, this transition takes place sometime between ages 16 and 21.
Typically, this transition takes place sometime between ages 16 and 21. 
